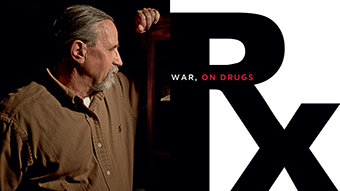
We see the staggering numbers, and yet somehow they don’t shock us nearly as much as they should.
Every day of the year in the United States, on average, 22 military veterans and active-duty personnel make the decision to kill themselves—an astounding military suicide every 65 minutes. More soldiers on active duty in Iraq and Afghanistan have committed suicide than died in battle. Recent government research has also found that female military vets decide to end their lives at six times the rate of other women. For women 18-29, it’s almost 12 times the rate of nonveterans.

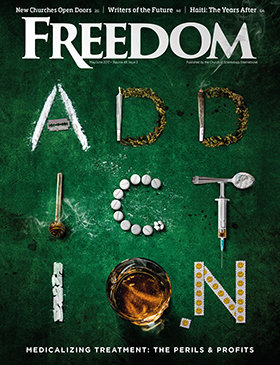
The culprit goes by the catch-all term Post Traumatic Stress Disorder, or PTSD, a convenient label that can efficiently house a laundry list of conditions generated in this case by combat stress. It might be chronic fatigue, depression, night terrors, or lingering pain. Overwhelmingly, the treatment offered soldiers and veterans centers on prescription drugs: antipsychotics, antidepressants, sedatives, stimulants and mood stabilizers.
Many have come to believe that this drug cocktail “cure” does significantly more damage than the condition it’s designed to treat, that it’s the narcotics themselves that have triggered an epidemic spike in veteran suicides.
Numbers tell part of the PTSD story, human tragedies tell the rest.
Military prescriptions for psychotropic drugs have soared 475 percent since 2002 and by 2014 stood at an astonishing 18 million annually. During that same period, the Department of Veterans Affairs opiate painkiller rate has climbed 270 percent.
Anyone serving on the front lines, it seems, can snare a diagnosis of PTSD. It happened to Mikal Vega, a 22-year special ops man who led Navy SEAL teams in Bosnia, Haiti, Iraq and Albania. During his first tour in Iraq in 2004, an IED (Improvised Explosive Device) detonated beside his Humvee, leaving him with a neck injury not immediately diagnosed, and mental anguish.
Within a week, Vega was seeing a psychiatrist and prescribed so many pills he couldn’t keep track of them all. Pills to stop the pain, stop the anxiety, to go to sleep, to wake up. Pills to cope. Pills to cope with the pills prescribed for coping.
“I know Prozac and Adderall were two of them, but I honestly can’t recall all of their names,” Vega admits. “The psychiatrist kept upping my medication and I’d feel more and more anxious. One day, I started feeling these chest pains. I couldn’t breathe. I was having drug-induced cardiac arrest. I thought I was dying. And that was OK with me, because it felt better than living. I just wanted to get it over with.”
Iraq War veteran Jody King can relate. While serving in combat, he was prescribed a mix of powerful drugs including the antidepressant Celexa, the sleep aid Ambien and the painkiller Tramadol.
“I was going around into combat oblivious of what was going on around me,” he said.
Eric Montalvo, a 22-year Marine Corps veteran and JAG officer who is now a lawyer focusing on military law, observed: “There’s no accountability for what happens with the dispensing of these drugs, which are potentially the biggest killers of all.”
How did it come to this? To understand why military prescription drug use skyrocketed, it helps to recognize that pharmaceutical companies collectively generate “a third of a trillion dollars a year as an industry,” says Col. Bart Billings, a retired Army psychologist and longtime advocate of nondrug therapies.
Billings tracks the beginning of the wildly lucrative psychiatry-pill conglomerate’s military relationship to a comment by the chief psychiatrist for the U.S. Army in the early 1970s. At the time, the psychiatric industry was in decline, looking for a reason to justify its existence. It needed to legitimize medical foundations for mental illness and to bring the pharmaceutical industry on board.
“Basically, what this Army psychiatrist said was that unless psychiatry did something radically different, the profession was going to go away,” Billings says. “The idea was that the old Freudian analysis takes too long, is too ineffective, and insurance companies weren’t going to pay for it. So psychiatry was on its way out. Then along came the pharmaceutical industry to say, in effect, ‘Hey you guys, if you can come up with the disease label, we can prescribe the drugs. It’s win-win.’ It was a matter of desperation meeting opportunity.”
In 1980 came the first listing of a “PTSD” diagnosis by the Diagnostic and Statistical Manual of Mental Disorders (DSM). Previously known as Soldier’s Heart, Shell Shock, Battle Fatigue and Vietnam Syndrome, PTSD was described as a “disorder” caused by “a traumatic event that involves actual or threatened death or serious injury.” The primary symptoms included “re-experiencing, hyper-vigilance and avoidance/numbing.”
What it represented more than three decades ago was an opportunity for drug companies such as GlaxoSmithKline, Pfizer and Eli Lilly and the pharmaceutical lobby that unites them to exploit this golden goose for extravagant profits. Fully one in five veterans who served in Iraq and Afghanistan have been diagnosed with PTSD.
Joyce Riley, a former Air Force captain, flight nurse and spokeswoman for the American Gulf War Veterans Association, cites the haphazard way veterans can be affixed with the PTSD label. She recalls the case of a serviceman who was diagnosed with PTSD, attributed to his mother’s death.
“The thing is,” Riley says, “his mother died when he was 12, and he was now a grown man.”
The side effects of these drugs are no secret. They range from mild dizziness, nausea, drowsiness, constipation and blurred vision; to mania, hypertension, hallucinations, psychosis; to heart attacks, stroke, suicidal ideation, and sudden death.
Fred A. Baughman Jr., a San Diego-based neurologist with more than 40 years of professional experience and an outspoken critic of psychiatric practices, believes that “the majority” of active-duty and veteran suicides can be traced to the rampant prescribing of antipsychotics and antidepressants. He also finds the PTSD diagnosis itself to be medically invalid.
“PTSD is simply another illusory, never-validated disease,” Baughman insists. “This is not to diminish the difficulties experienced by soldiers and veterans. But this is simply another way to represent purported “mental illness”symptoms and behaviors as a disease.”
Vega agrees with Baughman that PTSD isn’t an actual disorder but “a normal physiological response to abnormal conditions—which in the military means sustained periods of high anxiety.”
Jim Dolan, executive director of the Laurus Foundation, a nonprofit organization in Illinois dedicated to advancing the lives of individuals with disabilities, has another definition for PTSD, not as a mental illness but “a psychological wound” most effectively handled by first treating the body.
“Psychiatry has seen fit to turn PTSD into a cluster of symptoms used to categorize people,” Dolan says. “The trauma that results from combat is like that suffered by people in grief over a death. You need time to process the sorrow. Drugs tamp down the symptoms and do nothing to actually heal the trauma. Psychotropic medications essentially encourage a person to stop caring.”
What’s perhaps even more confounding about the plague of suicides is that fully half of those who took their lives were never deployed.
Where is the media mainstream in all of this? Why doesn’t it make a greater effort to call attention to the ways of a pill-popping military culture?
Rick Seaman—a Vietnam veteran, radio host, stunt-driving instructor and author of the 2015 memoir C.I.B. 1969: A Combat Infantryman’s Journey—finds the answer in conflicts of interest involving TV news.
“Don’t think for a moment that CNN and NBC News don’t know about this,” Seaman said. “The reason they don’t go after it is, look at how many pharmaceutical companies advertise on the networks. They’re not going to bite the hand that feeds them.”
Seaman maintains that he beat his demons on his own because he had no help from the “PTSD Lobby”—since that didn’t yet exist. He wasn’t victimized, he said, by “the ridiculous number of pills that [Veterans’ Affairs] passes out.”
Those pills more often than not are the result of veterans having grown addicted to their PTSD drug regimens while in active service for the Army, Navy, Air Force, Marines or Coast Guard. It has become part of a lifelong dependency created by the Department of Veterans Affairs as it has increasingly turned to psychiatry and mental health treatment over alternatives.
Indeed, the vast bombardment of psychotropics on vets has fueled a crisis at the VA over the past several years, one driven also by misconduct and deplorable treatment delays throughout the administration network. It culminated a year ago with VA Secretary Eric Shinseki’s resignation.
The VA scandal that erupted in April 2014 exposed a badly broken bureaucracy bloated with venality. It began with a report from Phoenix, Arizona, based on the testimony of Dr. Sam Foote, a whistleblower who called attention to an overburdened network clogged with patients forced to wait as much as a year or more for appointments. As veterans died waiting for critical care, the VA falsified reports and “cooked books” to cover up the abuses.
That led to revelations of systemic abuses, including a report that the VA was forced to pay out $200 million to grieving families for the wrongful deaths of nearly 1,000 veterans.
Dr. Foote, who retired last year, has no regrets over blowing the whistle. He only regrets that more hasn’t been done to remedy the situation since it came to light.
“They’re still not addressing the fundamental problem,” he stressed, “and that’s to look at the resources. They either need to downsize their mission or increase the funding to meet the greater demand. But Congress is willing to neither allocate more assets nor limit the scope of what they do. So it’s kind of business as usual, unfortunately.”
In the wake of the scandal, there has indeed been action taken toward reform in Washington. But the two recent pieces of legislation presented to that end are moving at a glacial pace.
A bill introduced in January by Congressman Gus Bilirakis of Florida, chairman of the Republican Policy Committee’s Task Force on Veterans Affairs, would allow veterans to receive alternative therapy and enable them to go outside the VA for whatever treatment they want. Called H.R. 4977, the Creating Options for Veterans Expedited Recovery Act (COVER), it provides $37.2 billion for veterans’ health care programs.
Congressman Bilirakis told Freedom that he developed the bill “because one size doesn’t fit all, especially when it comes to an issue as sensitive as the mental health care needs of our veterans. I have personally spoken to many veterans who have experienced dramatic results through the use of alternative treatments. I believe our veterans have earned the right to be active participants in determining their course of treatment.”
The suicide rate among veterans continues to alarm the congressman.
“When you have more casualties occurring with those who have proudly served here at home than overseas during their time of service, you have to ask yourself, ‘are we doing enough?’”
His bill is stalled at the committee level, as is a bill introduced in April by Congressman Jeff Miller of Florida, Chairman of the House Committee on Veterans Affairs. Called the VA Accountability Act, it would give the VA Secretary sweeping new powers to fire corrupt or incompetent employees for cause.
The VA itself announced last August an expansion of Patient-Centered Community Care (PC3) contracts that allow the VA to pay for veterans services provided outside of the VA itself. That too is rolling out sluggishly.
“Veterans have been complaining about these things for a long time,” notes Dr. Foote, “and finally their complaints have been more than validated. But awareness is still a long way from actually doing something about it.”
Part of the problem may well be that the VA has little incentive to change, given the fiscal windfall accrued from dispensing psych drugs—particularly when compared to unprofitable alternatives. The VA’s symbiotic relationship with the pharmaceutical companies, driven by financial considerations, takes precedence over the lives of service personnel they are duty-bound to care for, critics say.
The Los Angeles Times reported last year that disability awards for PTSD have grown nearly fivefold since 2001, and that half of those diagnosed may exaggerate or even fabricate symptoms to qualify for tax-free payments of up to $3,000 monthly.
The same L.A. Times article noted that PTSD disability payments have more than doubled to more than $49 billion since 2002, with the number of vets diagnosed increasing some 500 percent to more than 650,000 since 2001. It appears likely that the overwhelming majority of those receiving the PTSD label are peddled drugs and drugs alone as the magic elixir for their condition, real or imagined.
“What I’ve seen on a regular basis is just unbelievable,” says a self-styled veteran advocate and volunteer, who asked not to be named. “It’s literally a ‘No drugs, no money!’ thing. It’s criminal. What you wind up having is guys accepting the prescription and then tossing the drugs into the trash. The drugs are always the first consideration from the psychiatrists. Always.”
After leaving the service, Jody King remained on pills to relieve both physical injuries and mental impairment. But he found it impossible to find gainful employment due to the drugs’ effect on him. After quitting the meds and missing a VA appointment, he was threatened with decreased PTSD compensation. But he was OK with that. “There should be an alternative to taking multiple pills that don’t improve your health,” he argues.
There are alternatives. Proper diet and nutrition, vitamins, minerals, exercise, physical therapy—and many more. Service dogs provide companionship and help with everyday tasks and have been identified as an effective substitute for narcotics. But the big bucks alliance between the government and pharmaceutical companies virtually eliminates all motivation to promote or even mention them, explained a retired health professional who worked at a VA hospital for 28 years.
After his drug-induced cardiac episode in 2009, Mikal Vega picked himself up off the ground, stopped going to the VA hospital where he was being drugged, slowly weaned himself off the narcotics and began substituting natural therapeutic interventions that left him feeling good rather than near collapse.
Vega also founded the nonprofit Vital Warrior (www.VitalWarrior.org) that’s dedicated to building “decompression centers” designed to serve veterans with alternative therapies for healing body, mind and soul.
But he understands that it’s an uphill battle.
“Psychiatry has infiltrated the military to the point that they’re like gods,” Vega said. “Yet they hand out these little pills based entirely on guesswork and conjecture. And there are no consequences to them when they’re wrong. And when they’re wrong—which is often—people die.”