A 911 dispatcher’s voice flickers through the speakers. A SWAT team inches down a hotel hallway. Police radios crackle, then fall silent. Inside the Mandalay Bay shooter’s room a bottle of Valium lies beside a riot of crime-scene markers.
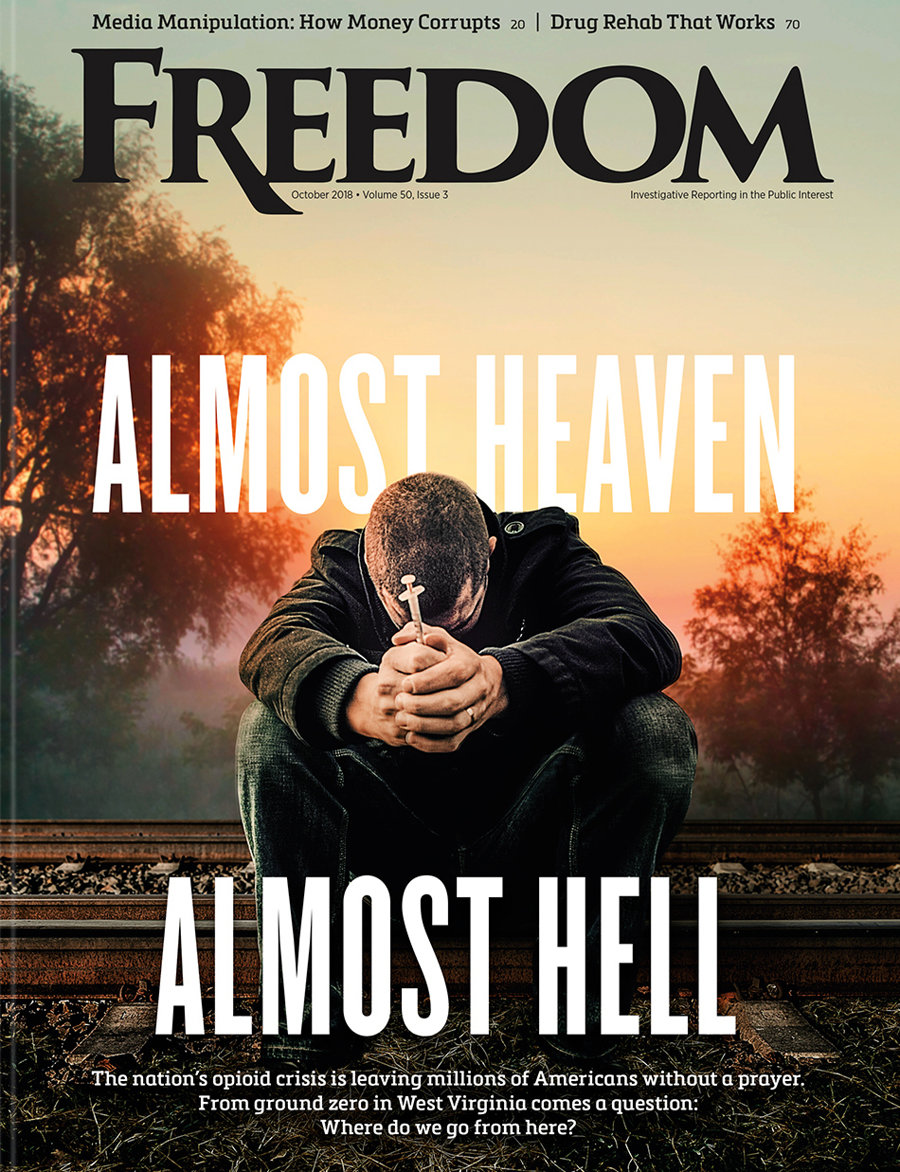
That 2017 collision in a Las Vegas casino—a mass killing and a neat, white-labeled psychiatric pill bottle—sets the through-line of Prescription for Violence: Psychiatry’s Deadly Side Effects, a new documentary from the Citizens Commission on Human Rights (CCHR), an international watchdog co-founded by psychiatrist Thomas Szasz and the Church of Scientology in 1969. The nonprofit is dedicated to investigating and exposing psychiatric abuse worldwide.
What the film makes unmistakably clear from its opening frames is that these drugs are not merely linked to private despair but directly implicated in public carnage. The Mandalay Bay massacre is aptly presented not as an anomaly but as the first entry in a grim pattern repeated across schools, malls, military bases and suburban streets: mass shooters whose psychiatric prescriptions appear again and again in the rubble they leave behind.
The autopsy found paroxetine in his system and nothing else. No other medications. No alcohol. No illicit drugs.
For CCHR, this territory is familiar. With chapters in more than 30 countries, the organization has spent decades documenting patient deaths, industry misconduct and the widening gap between psychiatric claims and psychiatric outcomes. Prescription for Violence extends that mandate, demonstrating that modern psychiatry’s most prescribed drugs have become a primary catalyst of suicide, violence and public harm.
What follows in the film isn’t a medical debate. It is an indictment—of the drugs, of the psychiatrists who prescribe them, of the regulators who approve them, and of the vast money system that keeps the machinery humming while families bury their dead.
Unlike suicides, mass shootings expose the public to the consequences of psychiatric drugging on a catastrophic scale. These are moments when private side effects become national news—impulsivity, aggression, dissociation, rage—and yet toxicology panels rarely test for the drugs most associated with those behaviors. The result, the documentary contends, is a public conversation about mass violence that misses a central vector: widely prescribed drugs capable of destabilizing judgment, amplifying hostility, and eroding the mental and emotional guardrails that prevent violent action.

The documentary threads this pattern through some of the most searing tragedies of the past decade. In Parkland, Florida, gunman Nikolas Cruz had been drugged since childhood, most recently with a cocktail including Risperdal, Focalin and Clonidine—drugs his own psychiatrist confirmed under oath. At Sandy Hook, investigators shielded the killer’s psychiatric records while simultaneously acknowledging that he had been treated by Yale-affiliated clinicians. In Dayton, Ohio, the shooter’s toxicology revealed benzodiazepines, including Xanax. Different states, different weapons, different victims—yet the same chemical through-line reappears again and again.
The film highlights further examples: the 2014 Fort Hood gunman, who had been prescribed antidepressants including Wellbutrin and Celexa; the Jacksonville video-game tournament shooter, who had been given the antipsychotic Risperdal; and the Nashville case of Kyle Craig, whose suicide after Adderall became a national warning about stimulant risks. Each incident, the filmmakers reveal, underscores the same blind spot: psychiatric drugs that can heighten agitation, impulsivity, paranoia and violent ideation, yet often go untested in post-crime toxicology.
By the time the film finishes mapping these case studies—Las Vegas, Parkland, Sandy Hook, Dayton, Fort Hood, Jacksonville—it becomes impossible to view them as isolated horrors. Instead, they comprise a single, national pattern: individuals destabilized by powerful mind-altering drugs that propel them into catastrophic violence, while regulators, prescribers and toxicologists look the other way.
After the scenes of mass violence, the film tightens its focus. One by one, individual victims appear on screen with stark captions: the drug, the date and a single word—suicide. The montage spans decades and continents, ending with a chilling three-word epitaph: “And countless others…”
The film’s argument is not that these individuals were doomed by their own minds. It is that they were caught in a pharmacological trap they were never warned about—prescribed psychotropics whose labels, inserts and sales pitches were crafted to minimize or conceal the very dangers that would end their lives.
The documentary then pulls back the curtain on an almost bureaucratic horror: the lack of testing for psychiatric drugs.
Investigator Gina Ross recalls combing through autopsy files and toxicology reports.
“One of the things that I used to do,” she says, “was to look at … drug tests all the time. And that’s just not something in my experience that’s routinely tested for.”
Trial attorney Andy Vickery pushes the point further and highlights additional cases: Standard tox screens simply don’t include the specific assays needed to detect most antidepressants.
“There’s a special test that needs to be done by a lab that’s certified to do that,” he explains. “Almost every time we have tested, we have found, yes, lo and behold, the drug is there.”
The implication is simple and staggering: The true scale of drug-linked violence—whether turned outward in homicide or inward in suicide—remains unknown, because the very chemicals that may have triggered those deaths are often never looked for.
If the drugs themselves are invisible in the lab work, psychiatry’s role is invisible in public discussion.
The film strings together clips of eminent psychiatrists repeating the same familiar propaganda: 85, 90, 95 percent of suicides occur in people with “pre-existing mental illness.” The profession’s response to every tragedy is to invoke the diagnosis, not the drug.
Lee Spiller of CCHR calls psychiatry “the invisible man.”
“The most you’re going to hear,” he says, is something like, “‘Oh gosh, I wish he had come into the office. I wish we had gotten to him sooner.’ You’re never going to hear, ‘Oh, yeah, that’s me, my drugs.’ Doesn’t happen.”
When suicides occur, the blame is redirected to the patient’s supposed “underlying disorder”—even when the person had little or no such history before his prescription was written.
Nothing illustrates this better than the story of Stewart Dolin.
Dolin was not a marginal case. He was a successful attorney at a major Chicago law firm, head of its mergers and acquisitions group, with no history of depression. He had some work-related anxiety. A doctor prescribed a generic form of Paxil.
Six days later, in sweltering summer heat, Dolin paced a subway platform he almost never used. Witnesses observed him walking back and forth, agitated, on the very edge of the platform. When the train finally thundered into the station, he jumped.
The autopsy found paroxetine in his system and nothing else. No other medications. No alcohol. No illicit drugs.
“This is a guy who had no business committing suicide,” says the family’s attorney, R. Brent Wisner. “He had the best years of his life ahead of him. It only took six days for the drug reaction to kick in and be so violent that he would commit suicide in that horrific way.”
GlaxoSmithKline’s own data shows that paroxetine multiplies the risk of suicidal behavior by more than six times.
Stewart Dolin never knew that. The label didn’t tell him. No one did.
If taking the drugs can drive a person into such a state, coming off them can be equally lethal.
Beneath many of these tragedies lies a word most patients have never heard: akathisia.
The film visualizes it as a woman in black limbo, splitting into multiple images, unable to stay put. The clinical definition flashes on screen: a movement disorder marked by inner restlessness, an inability to sit still.
But the clinical language doesn’t begin to capture the torment.
Victims describe feeling as if electricity, ants or fire are crawling under their skin. They pace, scratch, rock, writhe in bed. Their nervous systems feel “totally wigged out.” One man likens it to “internal torment … like hell.” Another, Josh Jensen, puts it bluntly: Akathisia “won’t kill you. It’ll make you want to kill yourself.”
Psychologist Linda Lagemann describes it as “intense, intense uncomfortable agitation that they can’t get rid of.”
The film presents the literature: study after study, across decades, linking antidepressants and antipsychotics to akathisia, and linking akathisia to violence and suicide. Pfizer’s own senior medical director once warned in a peer-reviewed paper that SSRIs—including the company’s own Zoloft—can make death “a welcome result.” He then wrote a memo advising the sales force not to discuss this with ordinary doctors.
No one in the film speaks about akathisia as a rare curiosity. It is portrayed as a predictable, if downplayed, effect of powerful psychiatric drugs—a “living hell” that can turn ordinary people into suicide risks and, in some cases, into sudden perpetrators of gruesome violence.
And if taking the drugs can drive a person into such a state, coming off them can be equally lethal. The film shows this through families blindsided by violent withdrawal: Rick and Kathleen Fee describing how their son went from honor student to threatening them during stimulant withdrawal, and Rory Tennes recalling how each drug change pushed him closer to uncontrollable aggression. Their stories make the film’s point unmistakable: The danger isn’t only in the taking—it’s also in the tearing away.
The film revisits mass shootings where perpetrators were in withdrawal: the Northern Illinois University gunman coming off Prozac; the Aurora theater shooter withdrawing from Zoloft; the Seattle Pacific University shooter tapering off Risperdal.
“These drugs are powerful, and our brains and entire bodies adapt to them,” explains psychologist Gretchen Watson. “And often people experience very serious psychiatric symptoms when they’re withdrawing.… That’s one of the riskier times also for violence toward self or others.”
Lagemann calls it a “withdrawal syndrome” built into every psychiatric drug. Defense attorney Kendra Parris adds that psychiatrists often avoid the word addiction by inventing a euphemism: “Discontinuation Syndrome.” The symptoms, she points out, look exactly like withdrawal.
The documentary is unsparing in its term for that cycle of reliance and withdrawal: a dependency trap. Drugs are prescribed, side effects appear, dosages are raised, and when the patient or family finally tries to stop, the system blames “relapse” and pushes them back on the same substances.
The film then makes a pivot from individual tragedies to the science that supposedly justified these drugs.
Harvard placebo researcher Irving Kirsch appears on-screen, offering his meta-analyses of antidepressant trials.
“The difference between the effect of a placebo and the effect of an antidepressant,” he tells 60 Minutes, “is minimal for most people.” If patients had taken sugar pills, he says, they would have experienced almost the same benefit—without the dangerous side effects.
The documentary lingers on that contrast: a chemically inert tablet that can make people feel better because they believe they’re being helped, versus a chemically potent drug that produces the same insignificant improvement, but with black-box warnings for suicide.
That contradiction—no measured benefit, life-altering harm—is where attorney Wisner enters the frame. He puts it in courtroom language: “Sugar pills don’t cause mass murders or suicides. These drugs do. If they’re no more effective than sugar pills, they shouldn’t be on the market. It’s an unacceptable hazard to human health.”
On top of that, the film notes, psychiatrists don’t even know how their drugs work. Package inserts admit, in dry pharmacology sections, that “the mechanism of action is unknown” or “presumed to be” some effect on brain chemicals.
“There’s no place for saying ‘presumed to be,’” says Lagemann. “That’s not science. Nothing should follow that. It should just be: ‘We don’t know.’ Period.”
The serotonin “chemical imbalance” story, long used in advertising to coax patients into accepting their prescriptions, is exposed as a marketing myth—finally dismantled in a 2022 umbrella review, decades after it was deployed. Psychiatric influencers now insist they “always knew” it was an oversimplification. Their patients rarely got that memo.
From there, Prescription for Violence turns its sights on government.
It profiles Dr. Thomas Insel, former director of the National Institute of Mental Health, who admits in a TEDx talk, that despite tens of billions poured into research, suicide rates have continued to soar. “This is a kind of confession,” he says. His job was to make progress; instead, one person now dies by suicide every 15 minutes in the US.
“I lost my daughter because a medication that was known to kill children was approved.”
For 27 years, psychiatrist Thomas Laughren oversaw psychiatric drug approvals at the US Food and Drug Administration (FDA). Wisner calls him “the godfather of modern psychiatric medications.” In deposition, Wisner says, Laughren effectively conceded that many of the drugs he approved do not work as well as advertised—yet he approved them anyway.
Under Laughren’s watch, 12-year-old Candace Downing was given a sample pack of Zoloft to cure the anxiety she experienced before school tests. There were no warnings on the sample pack. Her parents were not told about akathisia. Soon Candace began scratching her arms, complaining of itching, feeling “pins and needles” under her skin. One evening, she curled up on her father’s lap with her sister, laughing at Animal Planet. A short time later, her mother came home, climbed the stairs and found her daughter hanging from the bed.
At the time, Laughren lived in the same Washington, DC, suburb as the Downings. Their daughters had danced together as toddlers. He attended Candace’s memorial service.
Years later, when Candace’s mother testified about her daughter’s death at an FDA hearing, a network reporter tried to ask Laughren on camera about the case. He put his hand over the lens, ordered the crew out of the press room, and allowed them back only on condition they not say Candace’s name.
When he finally retired from the FDA, Laughren printed a new résumé: 29 years of experience approving psychiatric drugs, now available for hire as a consultant to pharmaceutical companies.
No regrets. No public reckoning.
“I lost my daughter because a medication that was known to kill children was approved,” says Downing. “How could you support the approval of a drug you knew was killing children?”
So if the science is absent and the risks are enormous, why does the system keep doubling down?
The film’s ninth chapter, “The Money Machine,” answers bluntly: Psychiatric drugging is extraordinarily profitable. Together, psychiatrists and drug companies promote pills as the first—and often only—response to distress. Psychiatrists dominate FDA advisory panels that green-light new drugs. Academic “key opinion leaders” stand on podiums, taking industry money to reassure colleagues that these products are safe and effective, including for kids.

Some individual psychiatrists, like Jeffrey Bostic, made small fortunes. According to federal prosecutors, Bostic pocketed some three-quarters of a million dollars from Forest Pharmaceuticals to promote Celexa and Lexapro, including to pediatricians, even after those drugs carried black-box suicide warnings for anyone under 25. Forest ultimately pled guilty to illegal promotion and paid more than $300 million in fines. But he kept his speaking fees, later publishing an article advising psychiatrists to target schools because, as he put it, “that’s where the kids are.”
Meanwhile, the four major psychotropic drug classes—benzodiazepines, stimulants, antipsychotics and antidepressants—each generate billions of dollars in annual sales. Altogether, psychiatric drugs gross nearly $50 billion per year, feeding a global psychiatric industry valued at well over $400 billion.
Psychiatrists, on average, earn more than a quarter of a million dollars annually. They write prescriptions in 86 percent of office visits. And when asked on camera how many patients they have actually cured, they laugh nervously or concede a single word: “Zero.”
“Here’s a simple fact,” says Lagemann. “No psychiatric drug cures anything.… Another fact: Every psychiatric drug has the risk of serious effects that could be life-devastating.”
The business keeps growing. The cures do not appear.
For all its data and regulatory exposés, Prescription for Violence is ultimately held together by the faces of people who loved someone, watched them unravel on a drug, and then had to plan a funeral.
Kim Witczak, whose husband Woody received Zoloft for insomnia and spiraled into night sweats, terror and depersonalization before hanging himself in the garage.
Kristina Kaiser, whose daughter, Natalie, was put on Zoloft for mild social anxiety and later died after showing classic signs of toxicity: wide-legged shuffling, uncontrollable itching, coughing up blood. Her psychiatrist later told her, via voicemail, that Natalie’s records had been “kind of, sort of” destroyed in an office flood—a flood that occurred only after her death.
Rick and Kathleen Fee, who locked their bedroom at night out of fear of what their own son might do once Adderall-induced psychosis took hold. They later found him hanging in his closet.
Mathy Downing, who has spent years telling Candace’s story so that other parents will see the word “akathisia” before it is too late. “I can’t save my own child,” she says. “But I can’t just stand by and watch people lose their children.”
The film treats these families not as anecdotes, but as witnesses—individuals delivering their testimony from a crime scene that just happens to be an exam room, a pharmacy counter or a suburban bedroom.
For all that, the last chapter of Prescription for Violence refuses to end on despair.
Derek Braslow, an attorney who has battled drug companies in court, believes the atmosphere is changing. As more evidence and stories come to light, he says, people can finally grasp that “drugs can have terrible effects on people.”
The film urges viewers to do three things.
First, report harms. In the US, the FDA’s MedWatch system allows patients and families to document side effects directly—data that can, over time, reveal patterns significant enough to force regulatory reform. Most consumers don’t know they can file such reports themselves.
Second, educate. Know the words: akathisia, withdrawal, black-box warning. Read the package inserts that quietly admit the mechanism of action is “unknown.” Learn how often withdrawal is mislabeled “relapse.” Listen to those who have lived through it. As Wisner puts it, the goal is not to take away help but to “clarify risk.” Once people understand the danger, demand for these drugs, he argues, will start to fall—and supply will follow.
Third, hold prescribers and institutions accountable. Bartenders, as investigator Gina Ross notes, can be held liable when they overserve someone who later injures or kills in a drunk-driving crash. Doctors who prescribe mind-altering drugs with known risks—and fail to warn—shouldn’t enjoy a special exemption from liability. Already, more than 40 percent of US psychiatrists have been sued for malpractice, many cases involving poor outcomes, drug errors or wrongful death. The film suggests that is not a glitch but an early sign that the public is beginning to understand who, in fact, is turning their loved ones into statistics.
The documentary also highlights activism: parents like Sheila Matthews, who successfully pushed for a Connecticut law preventing schools from coercing parents into drugging their children as a condition of attendance. It was the first such bill of its kind, and it now protects families statewide from psychiatric blackmail in the classroom.
In its closing minutes, the film returns to the question that hovers over every scene: How much longer can this continue?
Psychiatrist Pamela Shervanick, one of the few insiders willing to criticize her own field on camera, asks: “How many people have to die and suffer before we shift this?”
Diane Stein, of CCHR, is even more blunt: “It’s not going to change until someone says, ‘That’s it. We’re not going to be a party to murder.’”
Lagemann asks when society will finally “wake up and say, ‘Oh my God, we’ve been trusting the wrong person.… The suicides, the mass killings—it’s because of the psychiatrist, it’s because of their treatment.’”
And then there is Matthews, whose statement could be a subtitle for the film itself: “There’s no doubt in my mind that if society knew what is being withheld from them, game over—game over.”
The film’s last images show a courthouse wrapped in crime-scene tape, the words “STOP PSYCHIATRIC DRUGGING” emblazoned across the steps alongside a litany of side effects: suicide, mass murder, akathisia, psychotic reactions, homicidal ideation. Two words sum up the final outcome: “ZERO CURES.”
Over a ticking clock, the narrator delivers the final call to action: Join the Citizens Commission on Human Rights, speak out, take action, report harms, refuse to be one more “side effect.”
The address on the screen is short and direct: CCHR.org.
The clock keeps ticking as the credits roll, and the message could not be clearer: When the public finally sees what’s been hiding behind the prescription pad—the deception, the dollars, the deaths—the blind trust that sustains this industry collapses.
And once that misplaced faith goes, so does the power that keeps the system afloat.