Yet in a twist both jarring and emblematic, Acadia’s CEO has been promised a $1.8 million bonus, which will be paid in March 2026.
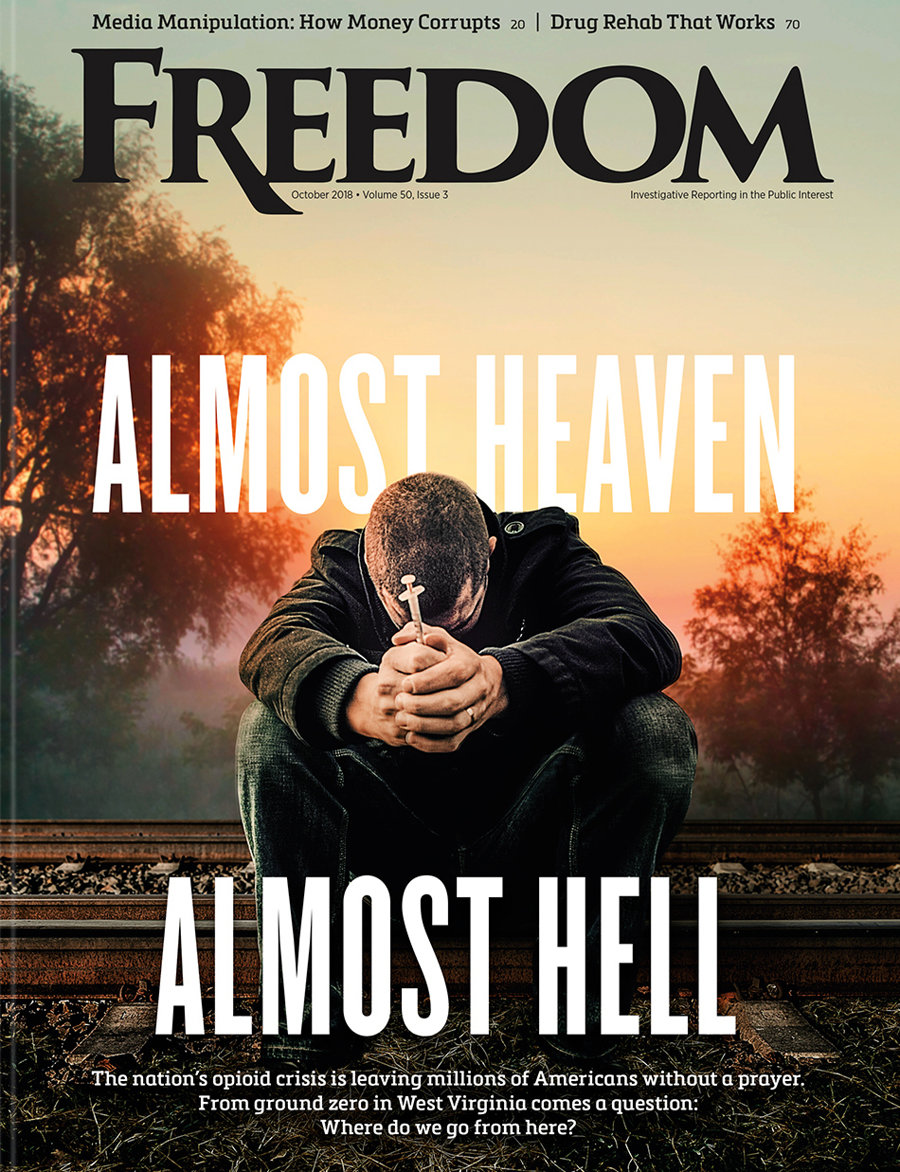
The unraveling of Timberline Knolls—and the broader misconduct allegations against Acadia Healthcare—casts a searing spotlight on the vulnerabilities of America’s abusive, profit-driven mental health system.
“The whole argument of tying your compensation to the stock price is so that the executives will bear risk of their actions.”
As for-profit providers step in to fill gaps left by public services, critics warn that Wall Street incentives can undermine care by rewarding executives even when their companies falter. At stake are the lives and safety of thousands of patients, many of them young, vulnerable and legally entrusted to these facilities.
Based in Tennessee and founded in 2005, Acadia Healthcare has grown into a sprawling empire: As of June 2024, the company operated 258 facilities across 38 states and Puerto Rico, tending daily to some 75,000 patients. Celebrities like Demi Lovato and Kesha once sought treatment at Timberline Knolls, lending it an air of prestige. But behind its wooded serenity, troubling signs began to emerge. In 2018, multiple residents accused a therapist of sexual abuse—allegations that marked the beginning of exposing a yearslong pattern of neglect, understaffing and preventable tragedies that would ultimately shutter the center in early 2025.
The 2018 scandal centered around four women who accused Timberline therapist Michael Jacksa of sexual assault. Instead of immediately alerting law enforcement, Timberline waited more than three weeks—only contacting authorities after the women filed complaints with the state’s substance abuse agency. According to court depositions, an Acadia executive allegedly instructed the facility’s then leader not to report the abuse. The case was quietly settled; Jacksa later pleaded guilty.
Although Acadia publicly pledged reform, it only intensified the very pressures that contributed to earlier abuses. Former staff say they were urged to fill beds, cut staffing costs and accept patients they couldn’t properly serve. “We were extremely understaffed,” said Cecilia Del Angel, a former aide. The patient deaths, she said, were “entirely preventable.”
Those deaths include 50-year-old Tiley McQuern, who fatally overdosed while staff reportedly failed to conduct required checks. Another resident, Deborah Cobbs, died after throwing herself down a staircase—just hours after multiple escape attempts and suicidal thoughts she vocalized. An unnamed foster child nearly died after overdosing on medication that had been left out in a common area.
Inexplicably, Illinois regulators did not investigate either suicide. Timberline existed in a gray zone—not licensed as a hospital or substance abuse center, and thus exempt from routine health department oversight. The state’s substance use agency hadn’t inspected the facility in six years.
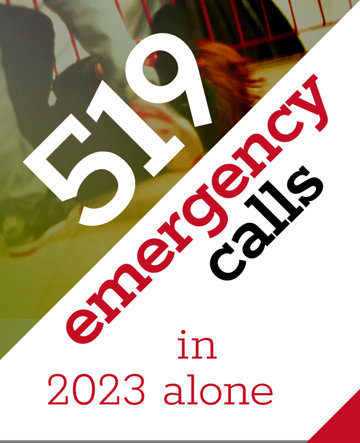
Meanwhile, the volume of 911 calls from Timberline surged—222 in 2020 to 519 in 2023—more than any other address in Lemont, Illinois. Acadia’s response? It’s because they “err on the side of caution,” in the words of spokesman Tim Blair.
Timberline is not an isolated incident. A 2024 New York Times investigation unearthed a pattern of abuse and neglect at Acadia facilities nationwide:
- A social worker was involuntarily held for six days at an Acadia hospital in Florida after seeking an adjustment to her drug prescription.
- A woman employed at a children’s hospital was involuntarily detained for seven days at an Acadia facility in Indiana after arriving to request therapy.
- 16 patients reported being held at an Acadia hospital in Georgia without explanation or valid reason.
Additional reported cases of abuse and neglect at Acadia facilities include:
- In Utah, over a dozen patients alleged sexual assault at an Acadia-run psychiatric hospital.
- In New Mexico, youth patients said staff coerced them into “fight clubs” and sexual acts.
- In Michigan, multiple women accused a former supervisor of sexual abuse, leading to a lawsuit involving over 40 survivors.
- At Acadia’s methadone clinics—the nation’s largest chain—federal investigators found the company billing for services it never gave.
Many of these cases are now under investigation by the Justice Department and the Securities and Exchange Commission. Yet the company, while losing roughly $5 billion in market value, has adopted a defiant tone.
“We reject any notion that we put profits over patients,” said Blair, adding that “complaints and incidents are investigated and addressed.”
And yet, as tragedy unfolded on the ground, the company’s executive suite reaped rewards. In 2024, CEO Christopher Hunter earned $7 million in compensation—plus a $1.8 million bonus tied directly to his management of the company’s legal woes. The CFO and general counsel each received $1 million bonuses, designed to ensure they didn’t leave in the face of federal investigations and the likelihood of shareholder backlash.
Critics like executive pay analyst Sarah Anderson of the Institute for Policy Studies call it perverse. “The whole argument of tying your compensation to the stock price is so that the executives will bear risk of their actions,” Anderson told The Times. “This is just going completely against that.”
No one illustrates the human cost more starkly than an 18-year-old former Timberline resident identified as J.P. In a harrowing lawsuit and interview, she recounted being groped by a staff aide, Erick Hampton, who was hired despite his history of domestic violence and gun charges. After reporting the abuse internally, nothing changed, she says. Hampton later lured her to his Indiana apartment, where she says he raped her repeatedly over the course of a week.
In August 2024, a second former patient filed a similar rape lawsuit. One official told reporters the facility “fell into a regulatory gray area.”
Class-action suits from shareholders, federal investigations and media exposés have battered Acadia’s public image. Yet its core operations continue. The broader issue, observers say, is systemic. For-profit psychiatric chains rely on high occupancy rates and insurance reimbursements to thrive, creating financial incentives to detain patients longer than necessary, admit those whose needs can’t be met, and reduce staffing to boost margins.
The shuttered Timberline Knolls campus now stands as a cautionary monument—quiet woods encircling an abandoned facility, stained with lawsuits and unanswered cries.
Meanwhile, Acadia Healthcare’s top brass remain at their desks, their bonuses locked in. The federal probes grind on. And the patients—many of them still healing, many others silenced forever—wait for justice that may never come.
Until there is meaningful reform, what’s disguised as “care” in these institutions will remain indistinguishable from harm—and the suffering will continue, sanctioned by silence. If history is any guide, systemic change won’t come until public outrage forces accountability.