Behind the festive warnings sits a broader reality: Illicit drug use remains widespread in England and Wales, and ketamine is increasingly visible within that landscape. The Crime Survey for England and Wales estimated that 8.7 percent of people ages 16–59 (about 2.9 million) used an illegal drug in the prior year, while around 1.1 million reported Class A use, the UK’s most dangerous category of drugs, including heroin and cocaine. Within that broader figure, ketamine use among 16–59-year-olds rose to 0.8 percent (up from 0.5 percent in 2015), and 16–24-year-olds reported 2 percent use in the past year.
Urologist Alison Downey told ITV News she is aware of colleagues treating patients “as young as 12 or 13,” calling the trend “shocking.”
What makes the current spike more than a familiar drug story is the age of the patients and the nature of the injuries. Doctors are describing urological damage that can escalate from pain and frequent urination to obstruction, kidney complications and, in the worst cases, reconstructive surgery or bladder removal.
Urologist Alison Downey told ITV News she is aware of colleagues treating patients “as young as 12 or 13,” calling the trend “shocking” and “very frightening,” particularly when so many tell clinicians they began using the drug “often in school.”
Downey’s clinical picture is consistent with ketamine’s core danger when used repeatedly. The drug’s anesthetic effect can mask the pain it helps create, while chronic use can inflame and scar bladder tissue—sometimes irreversibly—leaving young people with a daily life structured around toilets, cramps, bleeding and escalating medical intervention. “The impact that it has on these patients is horrendous,” Downey said, adding that early cessation can improve the odds of recovery, while later-stage damage can prove permanent.

Individual accounts put a human frame around what otherwise reads like trend data. In ITV’s reporting, 26-year-old Courtney Leggett described the humiliation that can accompany dependence—urinating in a bedroom bin to hide frequency, escalating to daily ketamine use within months, and eventually being told she would require radical surgery. “Having to have my bladder removed at 26 years old, it’s quite degrading in a way,” she said.
On the treatment side, providers say the holiday period can magnify risk, with parties, emotional stressors and peer dynamics converging when routines are already frayed. The UK Addiction Treatment Centres (UKAT) has warned that some ketamine clients as young as 18 spent the recent holidays in rehab. Zaheen Ahmed, a UKAT therapy director, said Christmas and New Year have become flashpoints for “binge” use and that people don’t understand the “long-term damage” or how quickly bingeing can slide into addiction.
The pressure is now visible inside Britain’s National Health Service (NHS) itself. In Wales, health board official Maria Evans told a council meeting that “in the last six months” the Royal Gwent Hospital had to create a “ketamine [treatment] pathway unit inside the urology unit” because of the number of people needing new bladders due to ketamine use—an institutional move that signals how rapidly the injuries are presenting and how specialized the response has become.
In England, the age curve has become so stark that Alder Hey Children’s Hospital in Liverpool opened what it described as the first NHS ketamine clinic for children and young people in the UK—built to address a rise in referrals for ketamine-induced uropathy (“ketamine bladder”). The hospital’s statement warned that damage can include ulceration and fibrosis of the bladder wall, with effects that “can be irreversible,” and that, in worst-case scenarios, might necessitate bladder removal or kidney dialysis.
In response to mounting harm indicators, the government has resorted to more direct youth-facing messaging. In October, the Department of Health and Social Care announced a campaign warning young people about ketamine and THC vapes adulterated with the substance. Health Minister Ashley Dalton emphasized that the choice to take drugs “can have profound effects,” and that ketamine “can destroy your bladder and even end your life.”
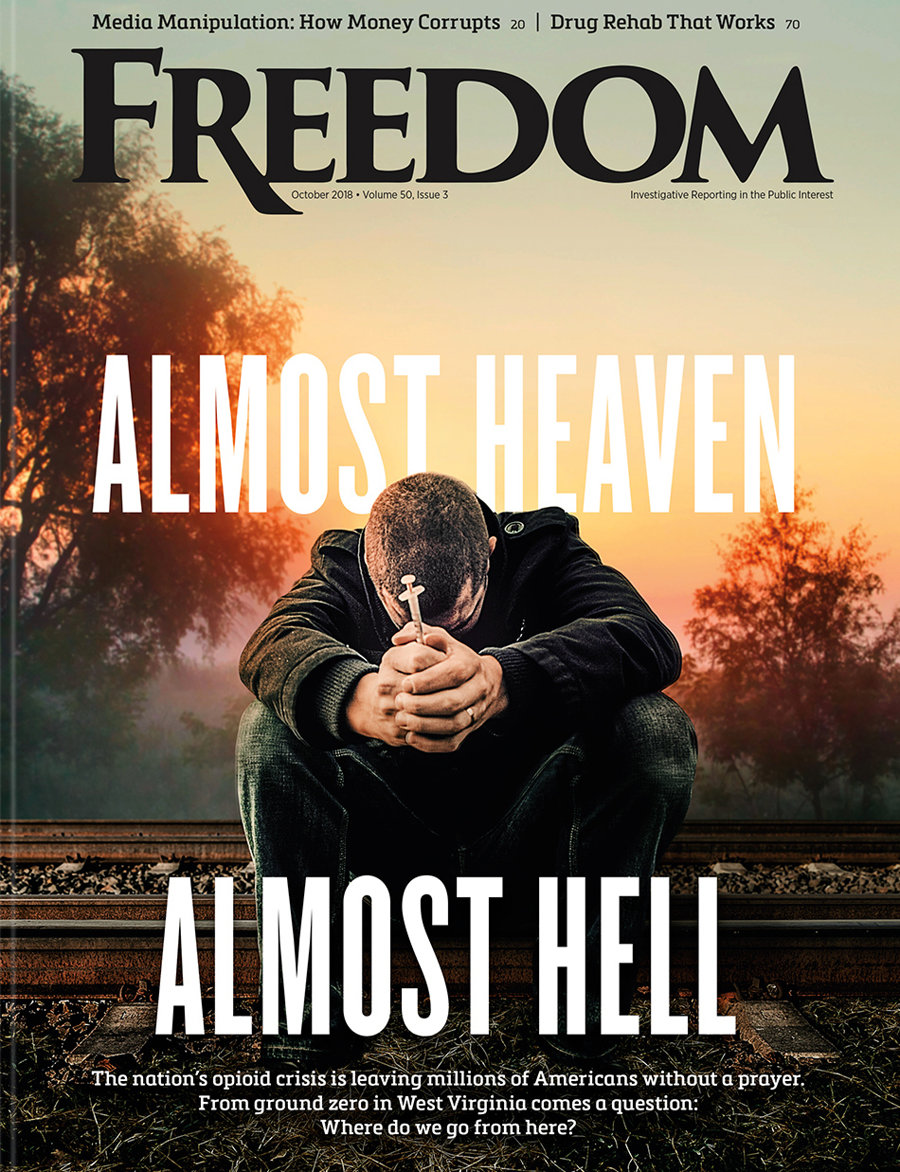
Freedom has tracked the broader arc of Britain’s ketamine problem through multiple reports in 2025—documenting the drug’s drift from nightlife experimentation into routine dependence, the illusion of “safer” use, and the way chronic injury can trap users in a self-perpetuating cycle of pain and relapse. The magazine’s earlier coverage has also highlighted how the crisis intersects with emotional vulnerability, cheap pricing and the speed at which severe physical injury can develop in younger users.
Amid these warning signals, prevention groups argue that education must be scaled to match the trend line. In the UK, Truth About Drugs campaign volunteers report at least 9,630 drug prevention events and distribution of more than 6.6 million booklets nationwide, including outreach in schools, transport hubs, shopping areas and nightlife corridors, as well as direct engagement with police and educators to support youth programs.
The next phase of Britain’s response will be judged less by how many headlines it generates than by what happens at the entry point—before a teenager becomes a urology case study. With clinicians describing school-age initiation, hospitals creating dedicated pathways, and government messaging turning more urgent, the question is whether prevention can move faster than normalization.
If it cannot, the country may enter 2026 with a bleak new baseline wherein ketamine harms are treated as routine seasonal fallout and childhood bladder damage becomes an accepted feature of the drug landscape—rather than the emergency it is.