The settlement framework, unveiled in January by New York Attorney General Letitia James and others, gained key support by June 16—paving the way for court approval of Purdue Pharma’s bankruptcy plan, which was filed with the United States Bankruptcy Court for the Southern District of New York in March 2025.
Payouts hinge on Purdue securing enough creditor support, which would let the company restructure and keep operating under court supervision. Funds would go to individuals, governments and Native American tribes, while the Sacklers would relinquish control of the 133-year-old drugmaker they have owned since 1952—the company they turned into a pharmaceutical empire whose legacy may be measured less in profits than in body counts.
“There will never be enough justice, accountability or money to restore the families whose lives have been wrecked.”
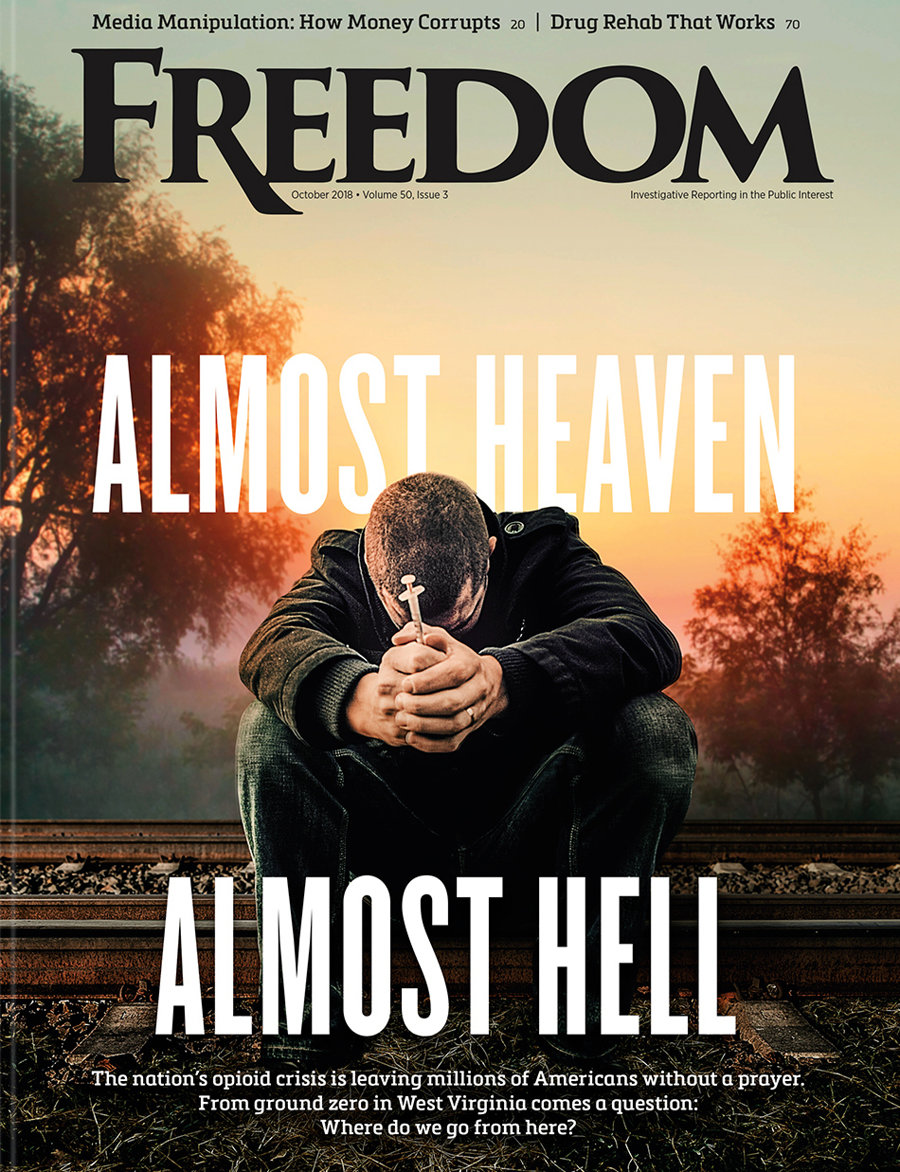
The deal, following years of lawsuits over Purdue’s role in fueling opioid addiction, is not merely another entry in the long ledger of corporate apologies. It is the final chapter in one of the most infamous pharmaceutical scandals in US history—and possibly the clearest example of how corporate greed, regulatory failure and medical misinformation collided to produce a man-made public health disaster.
Even as the Sacklers exit stage left with a multibillion-dollar payout, the government’s evolving response suggests that prevention has taken a back seat to emergency resuscitation. Narcan, the brand name for naloxone, has become Washington’s go-to life raft in the sea of opioid overdoses. Now available over the counter, the FDA-approved nasal spray, made by Emergent BioSolutions, is celebrated for reversing overdoses in progress—often within minutes.
But critics argue the drug’s prominence reveals a darker change in official thinking: rather than confronting the root causes of addiction, regulators appear more focused on rescuing the overdosed than preventing overdoses in the first place. In this reframing, the crisis isn’t the drugs themselves, let alone their deeper root causes. Rather, it’s the “inconvenience” of death.
The Purdue-Sackler settlement, which aims to settle allegations that OxyContin sparked a nationwide wave of opioid addiction, includes $6.5 billion from the Sacklers and another $900 million from Purdue Pharma. The money will be distributed over the next 15 years to fund opioid treatment, prevention and recovery programs, with more than half paid out in the first three years. California is set to receive up to $440 million, New York up to $250 million and Colorado around $75 million. If approved, the deal would push total opioid-related payouts by drugmakers, distributors and retailers past $50 billion.
“For decades, the Sacklers put profits over people and played a leading role in fueling the epidemic,” said Attorney General James. “While no amount of money can fully heal the destruction they caused, these funds will save lives and help our communities fight back against the opioid crisis.”
The agreement bars the Sackler family from producing, selling or marketing opioids in the US and ends their ownership of Purdue Pharma. A board of trustees, chosen by state attorneys general and other creditors, will now decide the company’s future under court supervision.
The road to this moment was anything but smooth. A previous $6 billion bankruptcy deal struck with the Sacklers was tossed out in June 2024 by the US Supreme Court, which ruled that it unlawfully shielded the family from future civil liability without the consent of all claimants.
Connecticut Attorney General William Tong offered a sobering assessment: “There will never be enough justice, accountability or money to restore the families whose lives have been wrecked or to right the terrible consequences of the Sackler family’s craven misconduct.”
By the time the FDA convened an advisory committee in 2002 to consider restricting approved uses for the drug, it was too late.
Purdue, for its part, struck a conciliatory tone, calling the unanimous support from states “a critical milestone” that will allow the drugmaker to deliver billions of dollars in compensation, and provide overdose-reversal drugs and treatment services. The company, now operating under court supervision, has even begun producing a new post-overdose medication, part of what critics describe as its final act in a grim cycle of harm and palliative.
But if Purdue and the Sacklers are the face of corporate culpability, federal regulators are not far behind. The US Food and Drug Administration (FDA) greenlit OxyContin for long-term pain use in 1995 despite scant evidence of its safety—a decision that helped launch the most aggressive marketing blitz in pharmaceutical history. Fueled by sales reps, promotional junkets and misleading claims about addiction risk, prescriptions quadrupled in less than a decade.
By the time the FDA convened an advisory committee in 2002 to consider restricting approved uses for the drug, it was too late. The majority of the advisers had financial ties to Purdue. Unsurprisingly, they voted to keep OxyContin unrestricted on the market.
OxyContin would go on to generate more than $35 billion in revenue for Purdue and the Sacklers. Meanwhile, overdose deaths soared, fueled first by pills, then by heroin, and now by fentanyl—a synthetic opioid 50 to 100 times more potent than morphine. According to the Stanford-Lancet Commission, a partnership between Stanford University and the respected British medical journal Lancet, another 1.2 million people could die in the nine years leading up to 2029 unless new interventions are implemented.
Despite that dire scenario, the FDA has never conducted a root-cause analysis of its failures and has resisted efforts to reform opioid labeling or approval practices, according to Andrew Kolodny, medical director of the Opioid Policy Research Collaborative at Brandeis University. Critics accuse the agency of embracing a pharmaceutical-first mindset, approving both addictive painkillers and the antidotes to treat the very overdoses they cause.
“Oversight bodies within the Executive Branch and Congress should conduct a long-overdue examination of the FDA’s role in the opioid crisis,” wrote Kolodny.
Added Kolodny, who is also president of Physicians for Responsible Opioid Prescribing, and has testified for states and counties in lawsuits targeting opioid makers and distributors: “Understanding why our regulatory systems failed to prevent a man-made epidemic is a critical step toward abating the opioid crisis and preventing future public health catastrophes.”
With this $7.4 billion settlement, the Sacklers may finally exit the stage, but their legacy—and the failures that enabled it—remain very much alive. The payout may help cities and states build the treatment infrastructure they so desperately need, but it does not answer the deeper question: How did a family become richer than the Rockefellers by selling addiction as medicine? And what does it say about the system that let them?
History will remember the Sacklers as profiteers of pain. Whether the institutions that empowered them will face a reckoning of their own remains an open, urgent question.