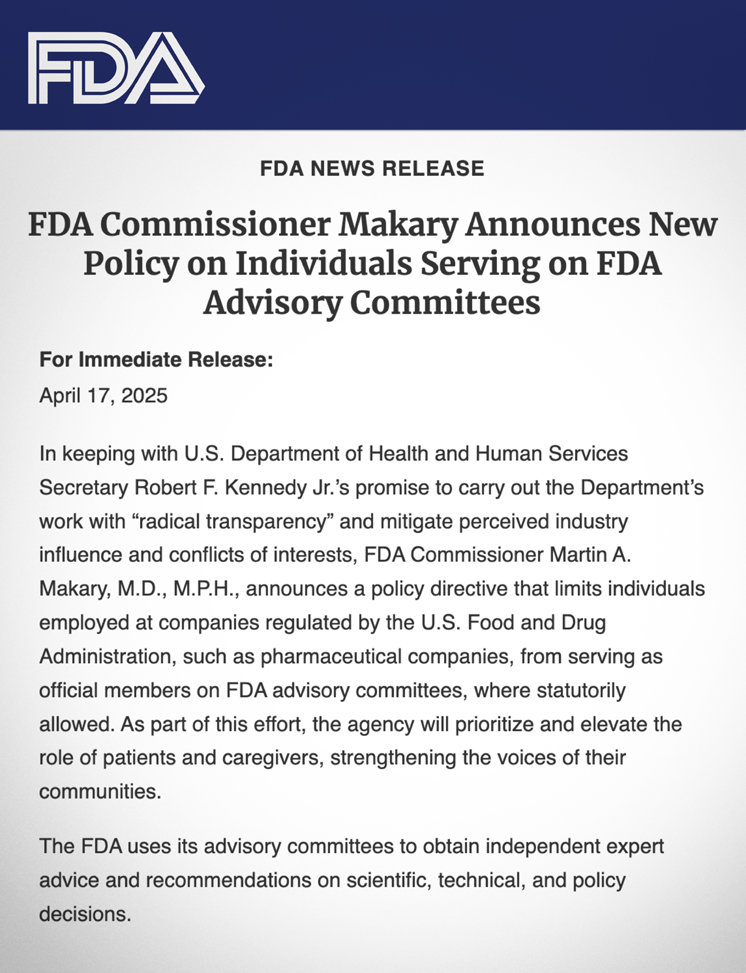
The directive, issued April 17, was framed by FDA Commissioner Martin Makary as a push for “radical transparency” to rebuild public trust and reduce conflicts of interest. In a news statement, Makary emphasized that, while collaboration with industry is important for a user-friendly review process, the scientific evaluation of new products must remain independent.
“Smart regulation” often looked like no regulation at all.
“Industry employees are welcome to attend advisory committee meetings, along with the rest of the American public,” Makary said. But appointing them as “official members [of FDA advisory committees] represents a cozy relationship that is concerning to many Americans,” the commissioner added, alluding to the FDA’s “history of being influenced unduly by corporate interests” and the fact that “public trust in the healthcare-industrial complex is at an all-time low.”
Makary reiterated his concerns on the platform X (formerly Twitter), underscoring the need for “impeccable integrity” in agency decisions. Under the new policy, patients and caregivers will be given greater prominence in FDA advisory panels, while industry representation will generally be limited to non-voting roles speaking for the sector as a whole—not for individual companies.
The backdrop to these reforms is a system that has, for decades, blurred the lines between public regulator and private profiteer.
Take, for example, the case of Patrizia Cavazzoni, who until January 2025 led the FDA’s Center for Drug Evaluation and Research, the agency’s powerful gatekeeper for new drugs. Cavazzoni oversaw a record-setting year of approvals in 2023, particularly favoring her former (and future) employer: Pfizer.
According to Fierce Pharma, Pfizer led the pack in what was described as a “bumper crop” of drug approvals under Cavazzoni’s watch—more than double that of its nearest competitor—just one year after the company posted record revenues of over $100 billion.
Cavazzoni’s re-entry into the executive ranks of Pfizer, where she now serves as chief medical officer, was lauded by the pharmaceutical giant. Pfizer hailed her “world-class” leadership in clinical development, regulatory affairs and drug safety, touting her accomplishments in “advancing public health initiatives” during her tenure at the FDA. But critics see her career arc as a glaring example of the “revolving door” that has long compromised the agency’s independence.
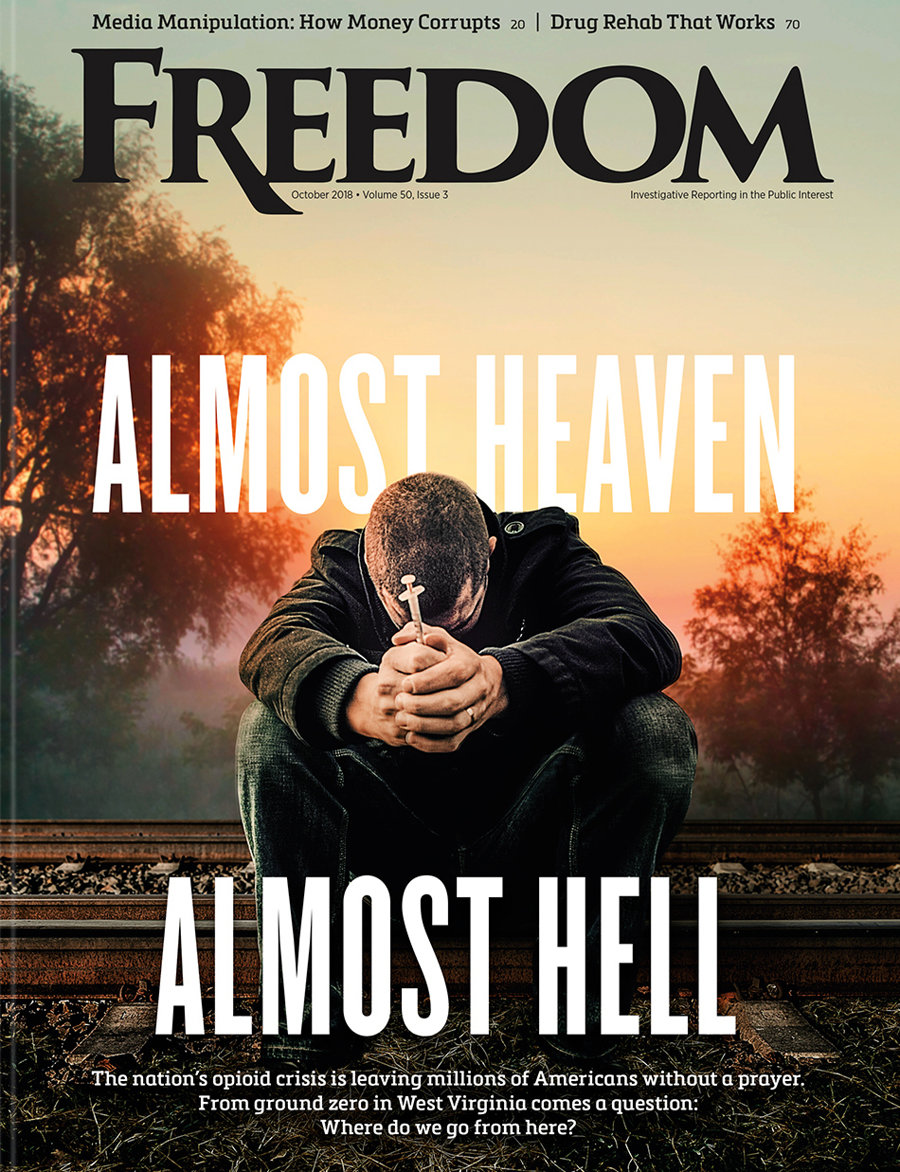
Pfizer, of course, is no stranger to controversy. As Freedom highlighted in March 2025, the company’s portfolio of psychiatric drugs—Zoloft, Geodon, Pristiq, Xanax, Effexor XR—has unleashed a litany of side effects ranging from anxiety and seizures to hallucinations, aggression and suicide, even as profits soared.
The incestuous relationship between the FDA and the industries it regulates doesn’t stop there. Consider the power couple Jeffrey and Allison Shuren. Until mid-2024, Jeffrey directed the FDA’s Center for Devices and Radiological Health (CDRH), the division responsible for evaluating the safety of medical devices. Meanwhile, his wife, Allison, co-chaired the Life Sciences and Healthcare Regulatory practice at Arnold & Porter, a powerful Washington, DC, law firm representing medical device makers and biotech companies.
As Freedom first reported in 2016—an exposé that The New York Times echoed eight years later—the Shurens epitomized Washington’s conflict-of-interest culture. Jeffrey’s tenure at CDRH coincided with aggressive defenses of lax regulatory standards like the 510(k) process, which allows medical devices to gain FDA clearance without new clinical trials if deemed “substantially equivalent” to existing products.
Such devices include electroconvulsive therapy (ECT) machines, which the FDA has classified as high-risk since 1976 but has never required to pass standard clinical safety trials. In 2011, Jeffrey Shuren proudly told the Senate that the FDA’s modernization efforts meant that US medical device makers dominated a $350 billion global industry. “Smart regulation,” not “more regulation,” was the goal, he insisted.
But “smart regulation” often looked like no regulation at all. In 2015, the FDA proposed downgrading ECT devices to moderate-risk, despite their long-documented hazards and despite the manufacturers’ repeated failures—dating back to 1979 and 1990—to submit required safety data. Under the Shurens’ watch, the FDA continued to protect corporate interests, leaving patients vulnerable.
Makary’s reforms represent a rare, perhaps overdue acknowledgment that the FDA’s credibility crisis cannot be solved by window dressing. The revolving door has been spinning for decades—and whether these changes slow it down remains an open question.