A new analysis from Quest Diagnostics—one of the nation’s largest clinical lab companies that runs millions of tests each year—examined more than 8 million workplace urine drug tests in 2024 and found that fentanyl positivity in random screenings was a stunning 707 percent higher than in pre-hire tests. Put another way: Job candidates can abstain long enough to land a position, but the nation’s most lethal opioid reappears once they’re on the job.
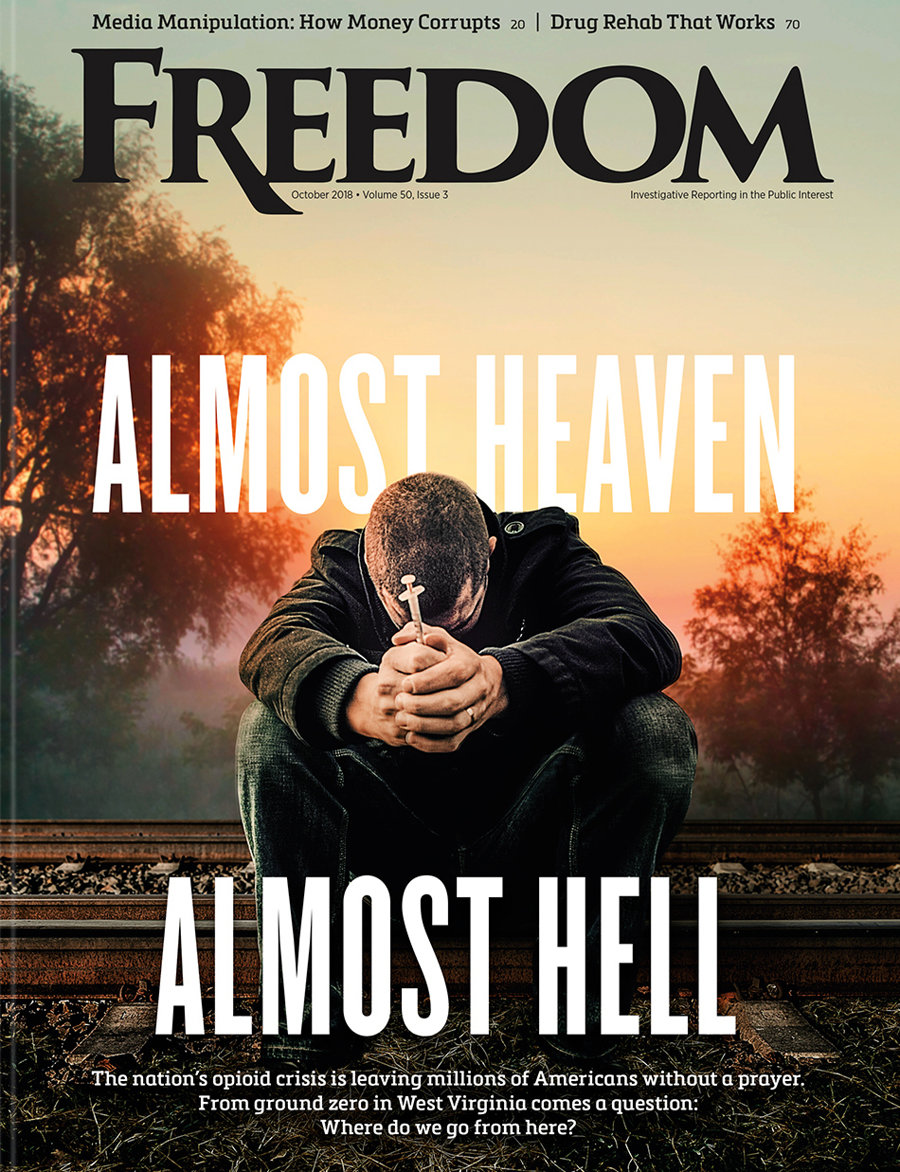
The opioid driving today’s overdose crisis isn’t just on the streets—it’s seeping into every corner of American life.
“Drug abuse is an ongoing issue among the American workforce.”
The gulf between pre-employment and workplace results has a simple but troubling explanation: fentanyl’s brief detection window, a quirk of chemistry that has become a loophole in workplace safety. Unlike marijuana, which lingers in the body for days or weeks, fentanyl clears quickly. Workers can stay off the drug for just long enough to beat a pre-hiring test—yet random checks expose them later. The effect is more than statistical. It shows how America’s deadliest drug is infiltrating everyday workplaces, with consequences for safety, productivity and public trust.
In 2024, overall fentanyl positivity among the US workforce hit 1.13 percent, up from 0.91 percent in 2023 and more than double the rate in 2020. Random testing revealed the starkest rise: 1.13 percent compared to just 0.14 percent in pre-employment screens. By contrast, marijuana positivity is typically higher in pre-hire than in random tests.
“The new Quest data indicates a worrying increase in fentanyl positivity in random drug tests as well as fentanyl drug-combing among the nation’s workforce in day-to-day work environments,” said Quest Senior Director of Science for Workforce Health Solutions Suhash Harwani. “It is disturbing to see increased use of fentanyl on the job and in combination with other drugs, given fentanyl’s extreme potency, which can increase risk of impairment, accidents and potential overdose.”
The Quest index also uncovered an alarming pattern of poly-drug use. Sixty percent of fentanyl-positive samples contained other substances. Co-positivity with marijuana has doubled since 2020, rising from 10 percent to 22 percent. Amphetamines also increased, from 11 percent to 16 percent. That mix heightens risks of impairment and accidents, particularly in safety-sensitive jobs like transportation, construction and healthcare.
Overall workplace drug positivity dipped slightly in 2024, falling to 4.4 percent from 4.6 percent a year earlier. Yet the rate has remained above 4 percent for a decade—evidence of a stubbornly high plateau. Marijuana remains the most frequently detected substance, at 4.5 percent, with post-accident positivity especially high at 7.3 percent. For-cause testing—ordered when supervisors suspect impairment—had the highest numbers, with one in three tests (33.1 percent) coming back positive in 2024.
“The overall drug positivity rate continues to reflect persistent trends,” said Quest Vice President and General Manager of Workforce Health Solutions Sam Sphar. “When we talk to employers, they tell us the same thing the Quest data tells us—that drug abuse is an ongoing issue among the American workforce. Many also realize that permissive attitudes around drug use can put their non-substance using employees, not to mention the general public, at risk.”
“It’s also concerning how fentanyl is showing up more and more in so many settings.”
Addiction specialists note that the workplace findings mirror what’s happening on the street. “This isn’t surprising,” said Steve Carleton, an addiction expert at Porch Light Health in Colorado. “It’s sort of based on what we know about drug trends and drug use.” Many bogus pills sold under other drug names now contain fentanyl, catching users unawares. As Carleton explained it: “When you’re buying substances on the street … you think you’re buying OxyContin, you think you’re buying a Xanax, which is a completely different type of drug, and really you’re buying fentanyl.”
Added Rob Valuck, a physician at the Center for Prescription Drug Abuse Prevention at the University of Colorado: “It’s also concerning how fentanyl is showing up more and more in so many settings.”
The federal Centers for Disease Control and Prevention has reported that seven out of 10 overdose deaths now involve illicitly manufactured fentanyls. After consecutive years of decline, fatal overdoses ticked up slightly in January 2025 compared to the year prior, underscoring the drug’s persistent danger.
Federal regulators are scrambling to catch up. Beginning July 7, 2025, the Department of Health and Human Services’ Federal Drug-Free Workplace Program added fentanyl to its testing panel. The Department of Transportation is considering similar changes. Meanwhile, Quest’s own data—compiled since 1988—has been used to guide federal workplace drug testing policy (the government’s Drug Testing Advisory Board was shuttered in March 2025).
What makes the Quest findings so unsettling is the way they cut across social perception. Fentanyl is widely seen as a “hardcore” street drug tied to cartel pipelines and overdoses. Yet the data shows its reach is broader and subtler, extending from job sites to cubicles, warehouses, classrooms, clinics and beyond. That contradiction is as much a cultural shock as it is a workplace hazard.
“It also raises concern that employees are turning to a dangerous drug like fentanyl after they’ve passed a pre-employment drug screen, putting the overall wellness of the workforce at risk,” Harwani noted.
Employers face hard choices. Many rely on pre-employment tests as their primary screening tool—largely to remain legally compliant—even though random testing often reveals a much higher rate of fentanyl positivity. But if fentanyl slips through at hiring, only to reappear in random screenings or post-accident tests, companies may need to reexamine their strategies—expanding random testing, providing support and tackling drug abuse head-on.
A 2017 National Safety Council survey of 501 managers at mid- to large-sized businesses found fewer than one in five felt fully prepared to tackle the opioid crisis. Only 13 percent were very confident they could spot risky use. Just over half said they screened all employees for drugs—yet 40 percent of that group admitted they didn’t test for synthetic opioids like oxycodone and fentanyl.
The larger point is unmistakable and urgent enough to bear repeating: Fentanyl isn’t just a street drug confined to the margins of society—it’s a workplace drug. Random tests keep uncovering what pre-hire screens miss—proof that the nation’s deadliest opioid has slipped past the front gate and into everyday jobs, revealing a cultural change that has blurred the line between “street problem” and “professional problem.”
And if the past decade’s overdose crisis is any guide, failing to confront fentanyl in the workplace may leave employers, employees and the public paying the price. The drug that once hid in alleyways is now hiding in plain sight—in the very jobs Americans depend on.